Recently I confronted consoling a affected person of mine who couldn’t perceive why I used to be unable to “hop on the telephone” to debate her new again ache. When she lastly acquired an appointment with me weeks later, I made a decision to be trustworthy. I shared that I had 1,300 sufferers who name me their main physician. After I’m accomplished seeing sufferers at 5 PM, I are inclined to 50 to 100 messages and notifications. I take three to 4 hours of labor dwelling with me each night time.
I didn’t share these stats to elicit sympathy, however quickly our roles had reversed. My affected person overflowed with apologies and demanded to know who was doing this to me.
That is the paradox that defines fashionable American medication: Medical doctors are working more durable and longer, all whereas sufferers can entry us much less. As a practising inner medication doctor and oncologist, I consider we reached this unsustainable state resulting from basically misaligned division of labor – between human and machine, between docs and help employees, and between what’s paid for and what good medical care requires.
As a health care provider, I’m no stranger to onerous work. However the methods docs’ workloads are exploding are largely clerical and bureaucratic. Paradoxically, an enormous wrongdoer is digital medical data. Paper data have been transformed to digital charts over a decade in the past, with the unimaginable potential to attach monumental quantities of affected person knowledge seamlessly. Nevertheless, the very know-how that was supposed to cut back docs’ work has drastically elevated it. Medical doctors right now spend two hours doing pc duties for each one hour dealing with sufferers. Ordering one thing so simple as Tylenol requires docs to click on between fourteen and sixty-two occasions, with the confusion inflicting errors in as much as 30 % of instances. The variety of clicks in a single ten-hour shift within the emergency room approaches 4 thousand. Practically 60 % of docs’ notes are an identical, and due to this fact redundant, to the earlier ones. The sensible result’s that docs spend hours digging by means of disorganized charts, sleuthing for essential affected person knowledge that will get buried below an avalanche of noise. In an period the place multibillion greenback software program guarantees to ease data-sharing, the method for suppliers to enter and discover well being knowledge stays guide, labor intensive, and error inclined.
Our present resolution to those technologic glitches is leaning on individuals to serve the wants of the digital charts. It was presupposed to be the opposite approach round. Help employees turns into essential, but patching logistical holes usually falls to docs. Just lately I prescribed a drugs that took 22 clicks, ready on maintain with an insurance coverage firm, monitoring down a denial letter, writing an attraction, documenting all these telephone calls, and holding my affected person apprised by means of messaging. What number of of these steps wanted to be accomplished by me? In my estimate, solely about half of my each day work really must be accomplished by an MD. The perfect run clinics perceive this and practice medical assistants to do way more than inventory clear robes and take important indicators. These clinics additionally rent nurses who can handle duties similar to refilling prescriptions, triaging affected person calls, and answering messages. However whereas staff help and delegation has caught on within the hospital setting, it lags in main care the place the physician usually performs all roles without delay.
Managing a affected person’s case on this fragmented system requires higher tech and staff help. It additionally requires time. In comes the ultimate mismatch: between what’s paid for and what medical care requires. Regardless of pushes in recent times for cost fashions that concentrate on worth, the overwhelming majority of well being care organizations within the U.S. nonetheless function based on fee-for-service. Right here, well being organizations or docs receives a commission based mostly on discrete companies they supply. In main care, that service has been commodified into the workplace go to. Nothing else instantly counts as paid work: not speaking with sufferers in between visits, not following up on take a look at outcomes, not digging by means of medical data, and never discussing instances with different docs. Furthermore, fee-for-service usually reimburses extra for visits with new sufferers than appointments with sufferers following up. With the monetary incentives stacked to guide as many sufferers as doable in face-to-face visits, appointments get compressed to fifteen minutes and a typical main care physician’s panel swells to over 2,000 sufferers. All the additional works spills into docs’ off hours. In the meantime, every affected person competes in opposition to hundreds for coveted appointments. When makes an attempt to safe well timed appointments fail, sufferers flip to messaging, transferring the deluge for docs to a different uncompensated channel that many practices are actually making an attempt to disincentivize by tacking on a cost.
The consequence is an ideal storm that drives good docs out of conventional medical practices whereas sufferers lose retailers to speak with them. I want I might have known as my affected person. However docs should choose their poison: they pace up and miss necessary particulars, spend their nights and weekends carrying over work, or go away. The choices for leaving embody going part-time (as a result of everybody is aware of the key that part-time is definitely full-time), becoming a member of concierge practices that cap at 200 sufferers in comparison with 2,000, or quitting medication fully. Sufferers who can’t get appointments navigate their very own lose-lose choices: they attempt to self-manage medical issues, flip to pressing care or emergency rooms for non-emergency points, or get billed once they ship messages asking for assist.
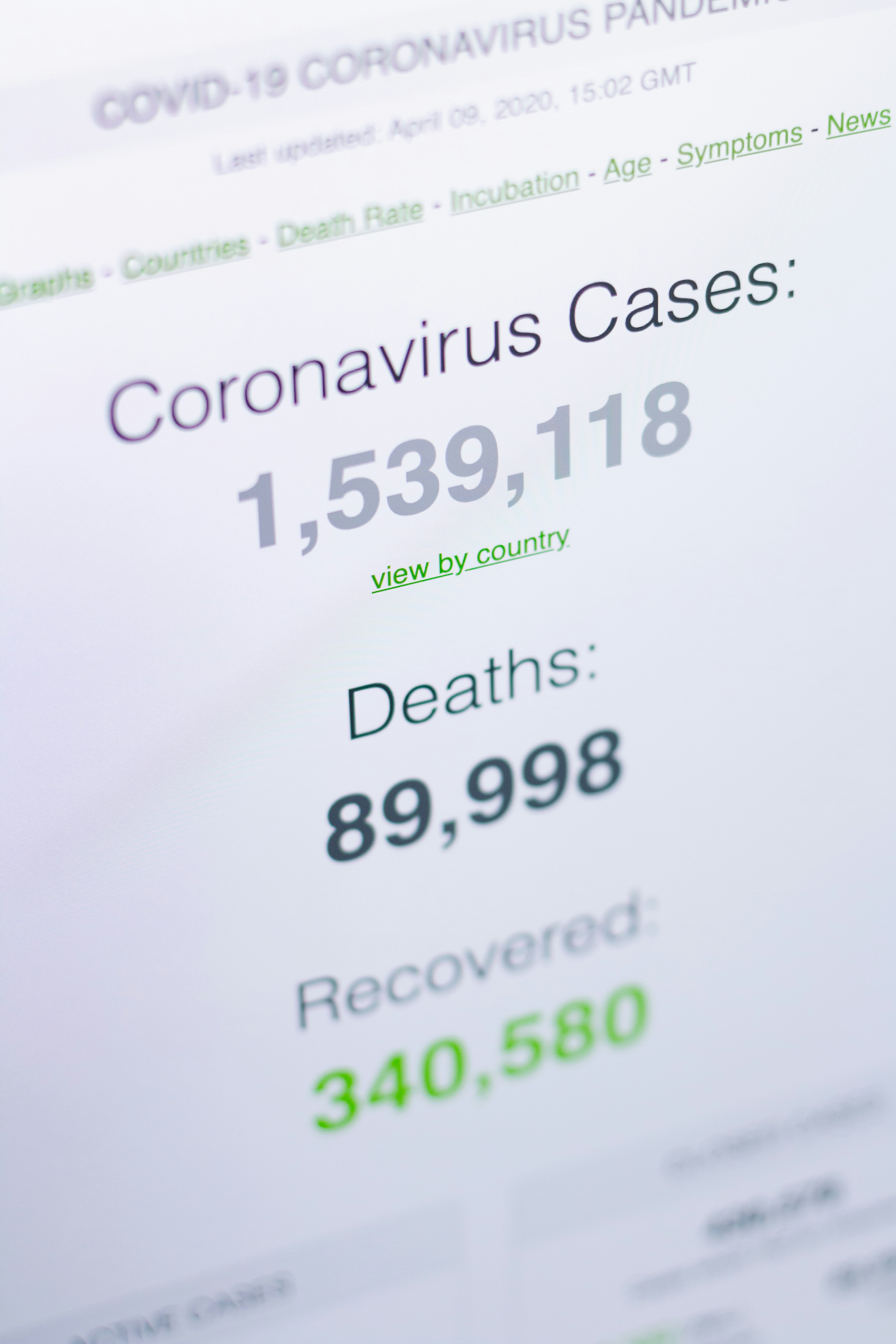
Fixing this disaster will contain profoundly rethinking how we allocate the sources we have already got. For years, the labor wanted to assemble disparate items of a fragmented well being care system continued to climb, whereas the celebration line to docs stays the identical: Only one thing more. Yet one more click on. Yet one more message. Yet one more workaround. Simply squeeze it in, we don’t know the way, however do it anyway, and do bear in mind if something goes fallacious the duty is totally yours. This mind-set is why main care docs are tasked with squeezing 26.7 hours of labor right into a single day. It’s why practically half of docs report burnout with bureaucratic calls for the number-one trigger (this stayed true each earlier than and through the Covid pandemic). And it’s partly why the common wait to see a brand new physician is 26 days and getting longer. Some fixes like altering cost fashions might be more durable to unfold. However different enhancements, similar to coaching employees to sort out clerical work and investing in high quality enchancment initiatives to reinforce the know-how, could be made now. With each proposed innovation, we should lastly take significantly the questions: Does this assist docs or make their lives more durable? Will this let docs know their sufferers higher or deepen the divide?
For a health care provider who has led life-and-death emergency responses to speak so fervently of paperwork and scheduling might sound ridiculous. It’s. However ignoring the mundane is how medication reached this untenable state; placing it off any longer is costing us time, power, and lives.
Extra Should-Reads From TIME